This is just my interpretation of available materials please feel free to share your ideas
ELSO operates multiple certification programs for extracorporeal life support (ECLS/ECMO) centers globally, with over 750 centers from 66 countries currently participating in their registry. The organization offers both institutional certification programs and individual practitioner certification, with a focus on standardizing ECMO practice and ensuring quality patient care across all age groups.
Certification Levels and Categories
Institutional Certification Programs
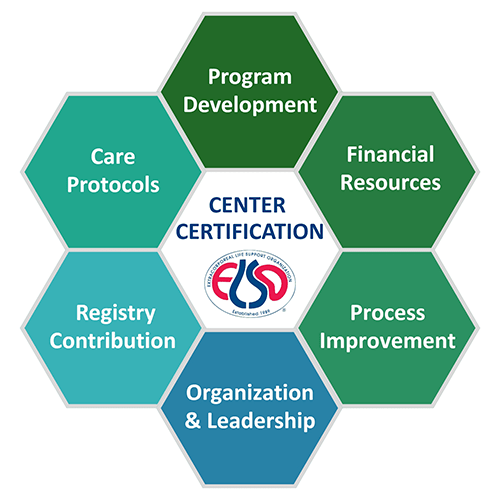
1. ECLS Center Certification
- Basic certification establishing global standards for ECMO/ECLS programs
- Addresses key components: team education, policies/procedures, governance, financial management, and research
- Valid for ongoing operations with renewal requirements
2. ELSO Award of Excellence (Center of Excellence)
- Three award levels: Silver, Gold, and Platinum
- Silver: Path to certification level
- Gold: Standard level of excellence
- Platinum: Highest possible quality of care (approximately 30 programs worldwide)
- Awards valid for 3 years with recertification required
- Recognized by U.S. News & World Report and Parents magazine
Patient Population Categories
Available certification types by age group:
- Adult ECMO programs
- Pediatric ECMO programs
- Neonatal ECMO programs
- Combined programs (treating all age groups)
Support type categories:
- Pulmonary support
- Cardiac support
- ECPR (Extracorporeal Cardiopulmonary Resuscitation)
Individual Certification
E-AEC (ELSO Adult ECMO Certification)
- Valid for 3 years with renewal required
- Open to MDs, NPs, PAs, RNs, RRTs, CCPs, and other healthcare professionals
- Includes NBME-style proctored exam
- Cost: $300 for 3-year certification
E-NPEC (ELSO Neonatal and Pediatric ECMO Certification)
- Currently in development/future launch
- Will follow similar structure to E-AEC
Eligibility Criteria
Basic Requirements
- Must be active ELSO member center
- Must participate in ELSO Registry
- Must demonstrate established ECMO/ECLS program operations
Award of Excellence Criteria
Centers must demonstrate excellence in three categories:
- Excellence in promoting ELSO’s mission, activities, and vision
- Excellence in patient care using highest quality measures, processes, and structures based on evidence
- Excellence in training, education, collaboration, and communication supporting ELSO guidelines
Application Process Steps
Pre-Application Requirements
- Critical first step: Review “Before You Apply” section
- Review ECLS Center Certification Methodology document
- Ensure active ELSO membership
- Assess initial eligibility criteria
Application Submission
- New centers only: Use new center application process
- Existing centers: Use renewal processes through member login portal
- Submit comprehensive application covering:
- Clinical activity documentation
- Quality control systems
- Training programs
- Patient/family support processes
- Pay non-refundable application fee at submission
Application Contact
- Center Certification: CenterCertification@ELSO.org
- Award of Excellence: award@elso.org
- General Support: support@elso.org | (734) 293-2101
Required Documentation
Core Documentation Areas
- Clinical Activity Records: Case volumes, patient populations, outcomes data
- Quality Control Systems: Policies, procedures, quality improvement processes
- Training Programs: Staff education records, competency assessments
- Governance Structures: Organizational charts, reporting relationships
- Financial Management: Budget documentation, resource allocation
- Research Activities: Current research participation, publications
Specific Requirements
- Established policies and procedures for patient care
- Comprehensive training and education documentation
- Family education program materials
- Quality initiatives and continuous improvement records
- 24/7 staffing capability documentation
- Equipment and supply management protocols
Staff Training and Credentialing Requirements
Key Personnel Requirements
Medical Director
- Overall responsibility for protocols, policies, education
- Must champion ECMO program to upper administration
- Responsible for patient selection criteria
ECLS Coordinator
- Designated position for training and education implementation
- Responsible for policies, procedures, quality initiatives
- Manages data collection and supplies
Staff Training Standards
- Comprehensive education processes based on ELSO Guidelines for Training and Education
- Formal training programs for all ECLS specialists
- Database entry exam required for all new centers and data entry personnel
- Ongoing competency assessment and continuing education
- Crisis support processes for staff after critical incidents
Individual Certification Requirements
- E-AEC prerequisites: Complete ELSO Foundations Adult ECMO course (53 modules, 80+ learning objectives)
- Clinical experience demonstration required
- Proctored certification exam passage
- Renewal every 3 years at $300 cost
Volume Requirements
Registry Participation
- Mandatory participation in ELSO Registry
- Continuous data collection across all ECMO runs
- Real-time validity checking for all data entries
- Minimum dataset requirements for all centers
Volume Considerations
- Centers grouped by volume for peer comparison
- Volume stratification used in quality reporting platform
- Volume factors into Center of Excellence status determination
- Over 190,000 ECMO runs currently in registry database
Quality Metrics and Reporting Obligations
ELSO Quality Reporting Platform Requirements
Mandatory tracking metrics:
- Survival rates
- Major complications
- Minor complications
- Length of stay
- Risk adjustment using published ECMO models (RESP, SAVE, PREP, Ped-RESCUES, Neo-RESCUERS, PIPER)
Data Collection Standards
- Real-time data entry with validity checking
- Database definitions manual with practical examples
- External validation of 10% random patient selection for Center of Excellence applicants
- Continuous quality improvement process documentation
Reporting Obligations
- Benchmark reporting against ELSO or peer groups
- Complication trend analysis (major, minor, patient, mechanical)
- Performance tracking across time with volume-based peer comparisons
- Registry data maintenance for quality reporting dashboard
Site Visit and Audit Procedures
Current Documentation
- Limited public information available about mandatory site visits
- Methodology documents provide detailed audit criteria
- Award of Excellence requires compliance with policies and procedures
- External validation component for Center of Excellence applicants
Evaluation Process
- Multi-focus assessment of ECLS centers
- Evidence-based evaluation of quality measures and processes
- “Above and beyond expectations” standard for Center of Excellence
- Annual compliance with established standards
Timeline for Certification
Processing Timeline
- Application processing time: Not specified in public documentation
- Review process: Involves comprehensive evaluation of submitted materials
- Decision notification: Through established communication channels
Program Timelines
- Award of Excellence: 3-year designation periods
- Terms expire: December 31st of designation year
- Individual certification: 3-year validity period
Renewal Requirements
Center Certification Renewal
- Separate renewal system from new applications
- Member login portal: “Login and click Manage, Renew Center Membership”
- Ongoing compliance with certification standards required
Award of Excellence Renewal
- Annual expiration: December 31st of designation year
- Reapplication required for renewal
- Continuous excellence standards must be maintained
Individual Certification Renewal
- 3-year renewal cycle for E-AEC certification
- Renewal process available through ELSO Academy
- Continuing education requirements for renewal
Costs and Fees
Application Fees
- Non-refundable application fee required at submission
- Specific amounts: Not disclosed in public documentation
- Fee inquiries: Contact support@elso.org or (734) 293-2101
Individual Certification Costs
- E-AEC certification: $300 for 3-year period
- Training courses: Costs vary by program
Additional Costs
- Registry participation: Included in membership
- Quality reporting platform: Included in certification
- Renewal fees: Contact ELSO for specific amounts
Program Benefits and Recognition
For Centers
- Global recognition of ECMO excellence
- Quality assurance to healthcare community
- Structured framework for program development
- Peer benchmarking capabilities
- Enhanced reputation and patient confidence
For Practitioners
- Standardized competency recognition
- Career advancement opportunities
- Global recognition of expertise
- Continuing education framework
- Professional development pathway
Key Contact Information
- Center Certification: CenterCertification@ELSO.org
- Award of Excellence: award@elso.org
- Training Programs: ecmotraining@elso.org
- General Support: support@elso.org
- Phone: (734) 293-2101
Conclusion
ELSO’s certification programs provide comprehensive standards for ECMO/ECLS centers globally, with emphasis on quality patient care, staff competency, and continuous improvement. The multi-tiered approach allows centers to progress from basic certification to recognized excellence, while individual certification ensures practitioner competency. Direct contact with ELSO is recommended for specific fee schedules, detailed procedures, and access to complete methodology documents, as some information is restricted to registered applicants and certified centers.