Introduction
Extracorporeal Cardiopulmonary Resuscitation (ECPR) is an advanced resuscitative strategy that combines conventional cardiopulmonary resuscitation (CPR) with the emergent use of veno-arterial extracorporeal membrane oxygenation (VA-ECMO) during cardiac arrest. Its goal is to restore circulation and oxygenation when traditional efforts fail. ECPR requires a specialized, multidisciplinary ECMO team, strict patient selection, and streamlined infrastructure. Recent European guidelines, as well as the integration of mechanical CPR devices and end-tidal CO₂ (ETCO₂) monitoring, are shaping modern standards of care.
Definition and Indications
ECPR is defined as the initiation of VA-ECMO during ongoing chest compressions for patients in cardiac arrest who have not achieved return of spontaneous circulation (ROSC). ECPR may be considered for:
Witnessed cardiac arrest with immediate bystander CPR Initial shockable rhythm (ventricular fibrillation or pulseless ventricular tachycardia) Short no-flow time (<5 minutes) and total low-flow time (<60 minutes) Reversible causes (e.g., myocardial infarction, pulmonary embolism, drug overdose, hypothermia)
Core Program Requirements and Criteria
1. Institutional Requirements
24/7 ECMO team availability Rapid response and transport systems Access to cardiac cath lab, interventional radiology, and intensive care services Integration with emergency medical services (EMS) and prehospital triage protocols
2. Team Composition
ECMO-trained physicians (intensivists, cardiothoracic surgeons, emergency physicians) ECMO specialists (perfusionists, nurses, or respiratory therapists) Support personnel: radiology, pharmacy, blood bank, and ethics committee
3. Patient Selection Criteria
Inclusion Criteria
Age: typically 18–65 (may vary by center) Witnessed arrest with prompt CPR (no-flow time <5 minutes) Initial shockable rhythm or signs of neurologically viable circulation (e.g., reactive pupils) ETCO₂ >10–15 mmHg during CPR (marker of adequate perfusion and likelihood of survival) Presumed reversible etiology Arrest-to-ECMO time goal: <60 minutes
Exclusion Criteria
Unwitnessed arrest Prolonged no-flow or low ETCO₂ (<10 mmHg after 20 minutes) Multi-organ failure or terminal illness Severe neurologic injury or DNR status Refractory asystole without reversible cause
Integration of Mechanical CPR and ETCO₂ Monitoring
Mechanical CPR Devices (e.g., LUCAS, AutoPulse)
Provide consistent chest compressions during transport, imaging, or cannulation Allow safe and uninterrupted compressions during ECMO cannulation Improve CPR quality, reduce team fatigue, and free staff for parallel tasks Now recommended by ERC (European Resuscitation Council) and ECLS guidelines as part of structured ECPR response
End-Tidal CO₂ (ETCO₂) Monitoring
ETCO₂ is a surrogate marker of perfusion during CPR Persistent ETCO₂ >10–15 mmHg suggests ongoing tissue perfusion and is associated with increased likelihood of ROSC and favorable neurologic outcome Sudden rise in ETCO₂ often precedes ROSC ETCO₂ trending is a key decision-making tool for ECPR candidacy
European Standards and Guidelines
The European Resuscitation Council (ERC) and European Extracorporeal Life Support Organization (EuroELSO) emphasize the following in their 2021–2023 updates:
Structured Inclusion Algorithms: Ensure rapid triage based on arrest setting, rhythm, CPR quality, and reversibility of the cause Prehospital Coordination: Implement prehospital alerts and direct transport to ECMO-capable centers Time Targets: Recommended arrest-to-cannulation time under 60 minutes; shorter intervals correlated with better outcomes Specialized ECPR Centers: Emphasis on centralized, high-volume hubs with simulation-trained teams, post-arrest care protocols, and outcome reporting Outcome Metrics: Programs should track neurologically intact survival (Cerebral Performance Category 1–2), not just overall survival
Role of the ECMO Team
The ECMO team functions as the operational core of any ECPR program:
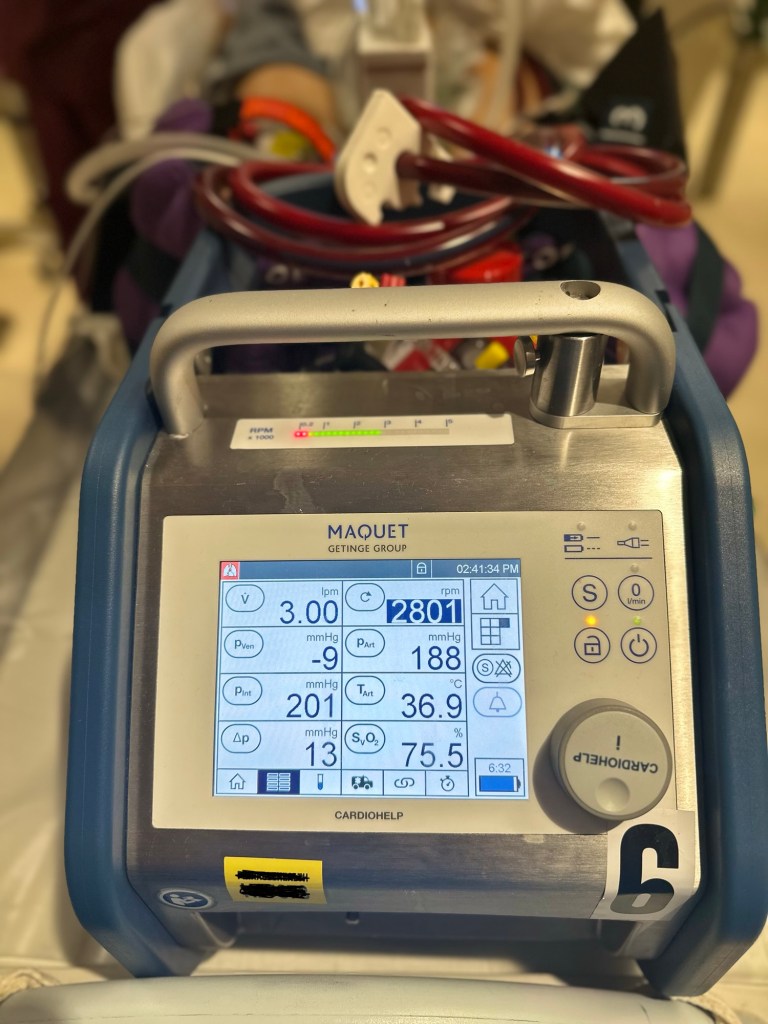
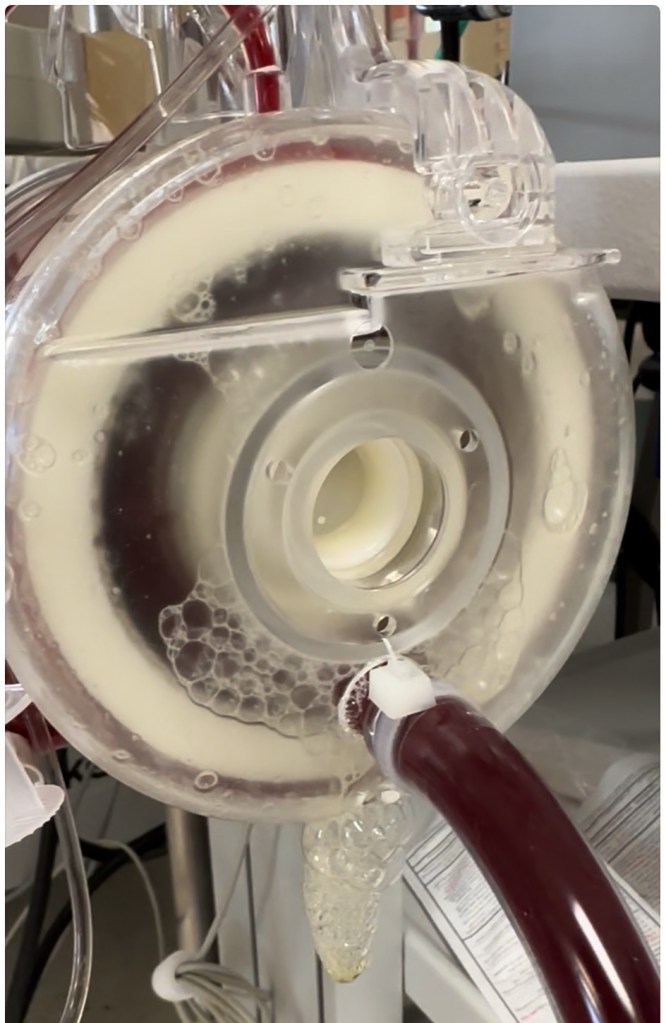
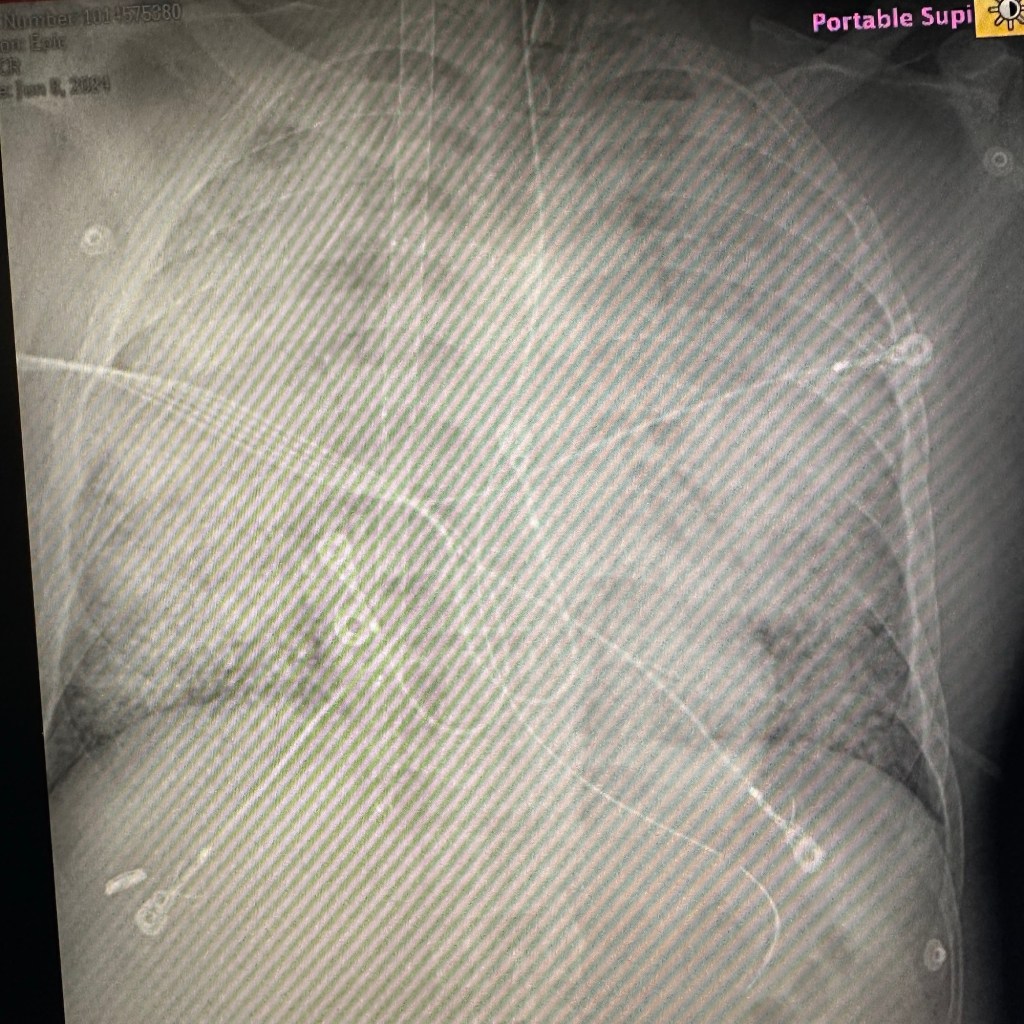
Initial Triage: Assess candidacy using protocolized criteria Cannulation: Perform rapid vascular access under mechanical CPR with ultrasound guidance Circuit Management: Initiate and titrate ECMO flows, monitor oxygenation and perfusion, manage anticoagulation Clinical Integration: Coordinate with ED, ICU, cath lab, and neurology teams Quality Improvement: Participate in debriefings, data entry (e.g., ELSO), simulation training, and process audits
Post-ECPR Care
Targeted temperature management (TTM) Immediate coronary angiography or CT imaging as indicated Neurologic monitoring and prognostication Daily evaluation for recovery or futility Ethical review and family communication protocols
Conclusion
ECPR is a high-resource, high-impact intervention with growing global support. Its effectiveness relies on fast decision-making, clearly defined protocols, and a skilled ECMO team. The integration of European best practices, mechanical CPR devices, and ETCO₂ monitoring has improved consistency, patient selection, and outcomes. As ECPR continues to evolve, ongoing investment in training, simulation, and quality assurance is critical to its success.